5 keys to improve adherence to exercise therapy
The demand for rehabilitation and physiotherapy services is increasing as the population ages and chronic, degenerative problems and other factors derived from current living conditions increase. This growth in demand generates saturation of services, as waiting lists increase, and as a consequence, so does the delay in receiving treatment.
Therapeutic exercise is the most effective treatment to treat any musculoskeletal injury, taking into account the long-term results. It is a fundamental clinical practice for the treatment and prevention of a large number of pathologies. However, the problem with these treatments where the patient is an active agent in his or her recovery is the lack of involvement in completing the prescribed exercises.
Much of the evidence in recent years takes as its reference the study conducted by Meichenbaum y Turk (1991), in which they proclaimed that one of the biggest problems in the therapeutic prescription of active treatments is the lack of adherence on the part of the patient. The study analyzed the failure rates in the follow-up of therapeutic prescriptions, in which short-term curative treatments had an adherence rate of 30%.
With the latter in mind and in order to combat this generalized lack of adherence to treatment, one of the most recent reviews published on the subject, the one conducted by Collado-Mateo D et al (2021), established a series of guidelines to increase adherence. From this study, we have drawn the following conclusions:
1. Protocolization and coordination
When establishing a therapeutic exercise treatment, we must ensure that the exercises are based on recent scientific evidence and quality. In addition, we must individualize them, so that they are adapted to the patient in terms of intensity, duration or frequency.
With respect to weekly frequency, it has been observed that exercise programs of 1 session/week result in poorer outcomes in therapy engagement.
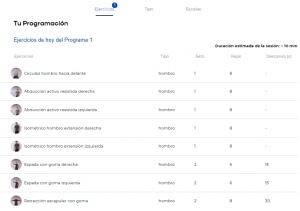
In the last blog post we talked about prescribing exercises for shoulder pain based on the patient’s typology. The treatment cycle recommended to offer the highest quality service to the patient is based on three main processes; customization, measurement and tracking and progression. It is essential to be able to to offer individualized treatments using simple scales such as the DASH scale, composed of 30 items. In this way we can guarantee patient safety by being able to prescribe treatments that are adapted to them.
Bei P et al, stated in 2018 recently that any exercise protocol increases adherence if the patient is supervised and monitored while performing it versus uncontrolled groups.
On the other hand, Sasan A et al recommended in 2020 the use of web applications that do not involve the patient’s presence. This is why the main calling card of TRAK is the supervision of exercise programs remotely, giving the patient flexibility to carry out his or her protocol.
2. Initial evaluation and monitoring.
We must always make an objective assessment of the patient’s own characteristics. Each person who comes to our clinic is different, so we must analyze not only the pathology they bring with them, but also their general health and lifestyle in order to find out how to increase their adherence to the protocol we have prescribed.
There are many negative factors associated with patients’ lack of adherence to treatment, such as sedentary lifestyles, smoking and the presence of chronic diseases, which are often related to situations of fragility or depression.
With regard to monitoring, the follow-up of the patient’s progression must be carried out with objective data that support the patient’s evolution. For this, there are indicators that we can use different mechanisms that we can use as a reference. On the one hand, through clinically validated scales and questionnaires, we can perform periodic assessments of the patient’s functional status. On the other hand, we can draw on objective metrics of the patient’s sessions and compare how they progress over time.

The Trak tracking system allows us to record the maximum range of motion per exercise, the number of repetitions performed, the execution time and many more indicators. These data allow us to know the functional improvement that the patient is getting in the different variants: pain, mobility, resistance…
3. Education and integration
Explain the benefits of exercise to the patient, the patient’s ability to see the benefits of any treatment will provide him/her with confidence in the treatment and also in the professional who is prescribing it. We must understand that either by habit (because of prescribing rest) or simply because he/she adopts an antalgic attitude, the patient continues to see exercise as something that can worsen his/her clinical situation.
It is not a matter of giving them a symposium on the benefits of exercise in the long or short term or on physiology, but in making them understand that therapeutic exercise is their new medicine, in this case. So we must get them used to working in a low pain setting and make them understand their pain so that it does not limit them. This will be key in ensuring their adherence to the program we have delivered.
There are many scientific articles that relate a high adherence to an exercise program with a correct inclusion of physical exercise in the patient’s daily life. Performing their protocols in an environment familiar to the patient, such as their home, and knowing that they are being monitored by a healthcare professional, reinforces this fact.
Face-to-face attendance involves certain difficulties that present themselves as problems for adherence, such as having to travel or the weather. In addition, adherence will be higher if it offers time flexibility and does not require attendance at a pre-arranged session.
4. Fluid communication and information between the professional and the patient
We have already seen that monitoring and supervision of the treatment, as well as constant communication with the patient is essential for him/her to feel motivated and adhere to the exercise program.

At TRAK we are aware of these concerns and therefore we offer the possibility of establishing direct communication with the patient with which we can generate an active interaction that will help him/her to comply with the prescribed treatment. It is important to transmit positive messages and even feedback on how to perform the prescribed exercise sessions.
It is also essential that, after several weeks of home work, reinforcement sessions are included for a more exhaustive evaluation to observe the progression, keep motivation high and be able to make modifications in the execution of the exercises or in the program itself.
TRAK provides both the healthcare professional and the patient with data on the progression of the treatment in a system of evolution graphs. It presents joint ranges, pain scale or adherence data to ensure that the professional obtains as much information as possible and the patient is motivated to continue to monitor their progression.
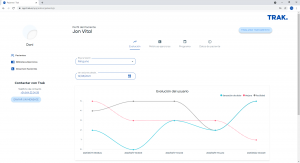
In addition, TRAK uses gamification mechanics that involve the patient in the treatment and can report the progress being made in a fun and attractive way. As can be seen in the image, we visualize the evolution that is being made 📈, you can earn Trak points💯 and have a record of the sessions held⚡.
5. Patient participation and targeting
Digital health is becoming more and more a reality, and one of its maxims is the empowerment of the patient and his valuation as an active part of his own treatment. This is stated by the WHO in the Proyecto de estrategia mundial sobre salud digital 2020–2025 and in the Proyecto REHAB 2030.
The patient must know, understand and become involved in his or her own treatment and for this purpose he or she must be informed, educated and offered self-treatment strategies that allow him or her to control part of the treatment.
Likewise, it is important as professionals that we organize our treatment and our protocols based on a series of objectives that are real and that are tailored to each patient.
Currently, there are tools available to offer tele-rehabilitation services with real-time assistance that allow objective monitoring of the patient’s evolution remotely.
If you want to know more about the advantages that TRAK could give you, don’t hesitate to request a trial!
Join digital rehabilitation!